DISCOLUX CERVICAL PLDD: Minimally Invasive Laser Treatment of Cervical Hernia.
Description:
|
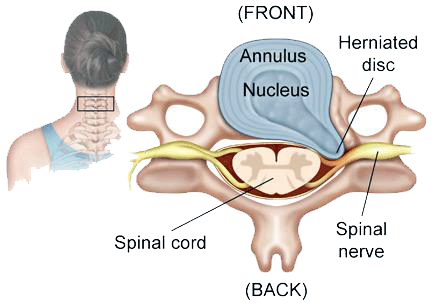
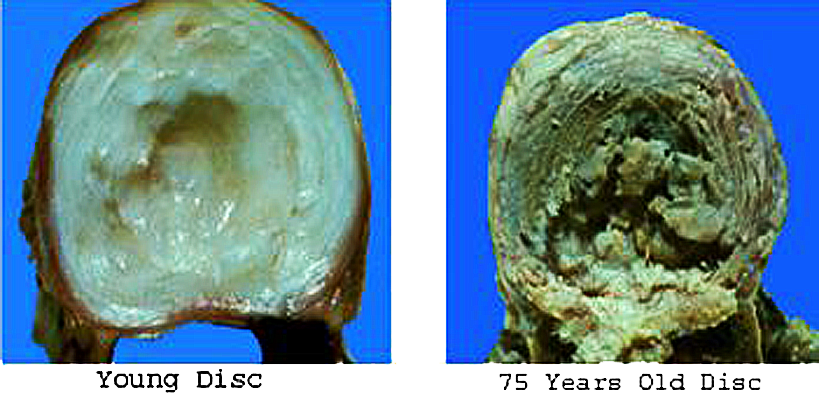
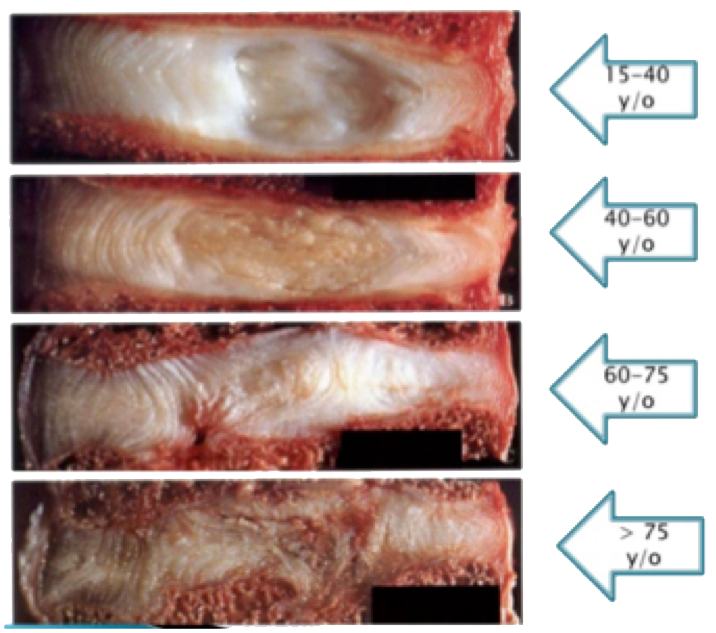
Cervical Herniated Disc, like the lumbar ones, is caused by a degenerative process on the disc / vertebral complex.
|
 |
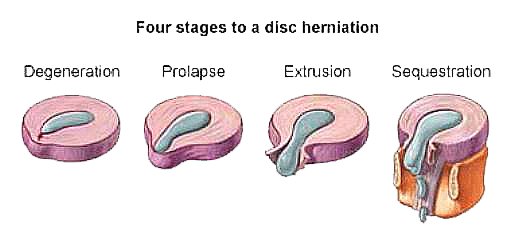
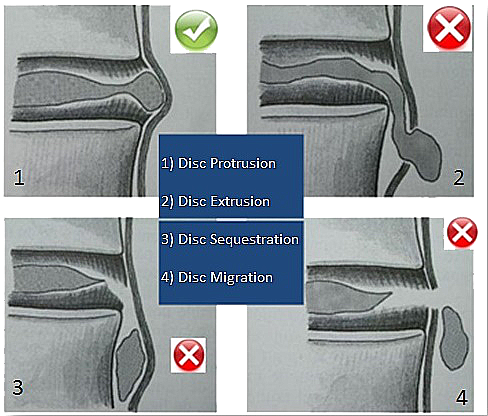
| Disc hernia is classified according to the disc herniation degree. • Degeneration: intervertebral disc aging, resulting in disc thickness loss and subsequent alteration of its basic biomechanical properties. • Protrusion: the disc loses its original consistency and its ability to amortize the loads of the vertebrae: deforming, it protrude, invading wrong spaces, for example by touching the nerve roots, but remains contained in the fibrous annulus. • Extrusion: the nucleus pulposus comes out by piercing also the longitudinal back ligament. • Sequestration: part of the herniated disc material is completely expelled and loses continuity with the nucleus pulposus; Sequestrated disc, corresponds to extruded disc material that has no continuity with the parent disc and is displaced away from the site of extrusion. |
 |
Symptoms of a herniated disc can vary depending on the location of the herniation:
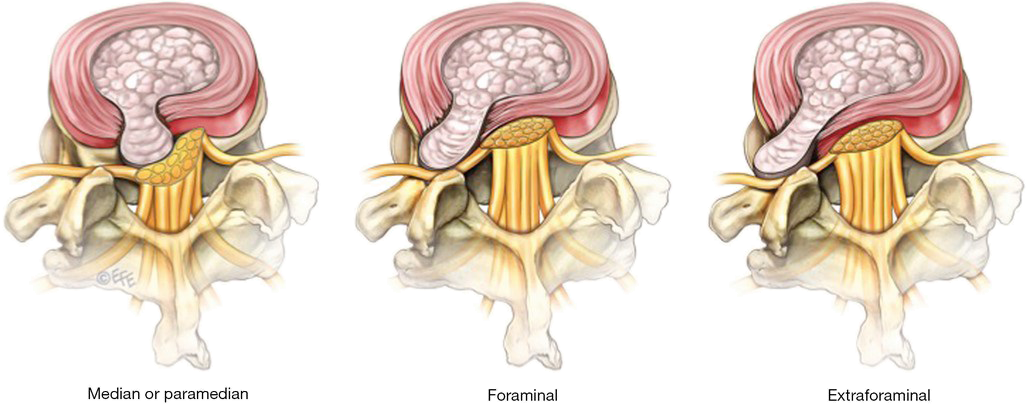
o Median: The hernia is located at the rear along the median line.
o Paramedian: The hernia is located at the rear not far from the median line.
o Lateral: The hernia is located at the rear, considerably distant from the median line.
o Intraforaminal: these herniations affect the intervertebral foramen, the nerve root is not only compressed and dislocated, as in the most common paramedian hernia, but also crushed against the vertebrae peduncle above and / or against the interapofisarias joint.
o Extraforaminal: these herniations does not affect the intervertebral foramen, but compresses the outer part of the nerve root at the exit level from the intervertebral foramen, or affects the overlying root if it is lateral.
Risk factors:
In addition to wear caused by aging, other factors may increase the disc hernia likelihood:
• Irregular posture of the back. Using back muscles to lift heavy objects without bending your knees can cause a disk hernia for the strong pressure exerted on the intervertebral discs.
• Gender. Men between the ages of 30 and 50 are more likely to have a hernia.
• Weight. Being overweight adds tension on the back disks.
• Repetitive activities that strain the spine.
• Many jobs are physically weary, some foreseeing continuous lifting, pulling, flexing or twisting.
• Driving for long periods. Vibrations put pressure on the spine and discs.
• Sedentary lifestyle. Regular exercise is important in preventing many diseases, including a disc hernia.
• Smoking. Smoking cigarette is believed to reduce oxygen supply to the disc and cause faster degeneration.
• Cervical hernia may be caused by road accidents that cause whiplash or other trauma.
 |
 |
Symptomatology:
Symptoms of a cervical hernia are many, ranging from asymptomatic hernia to paralysis.
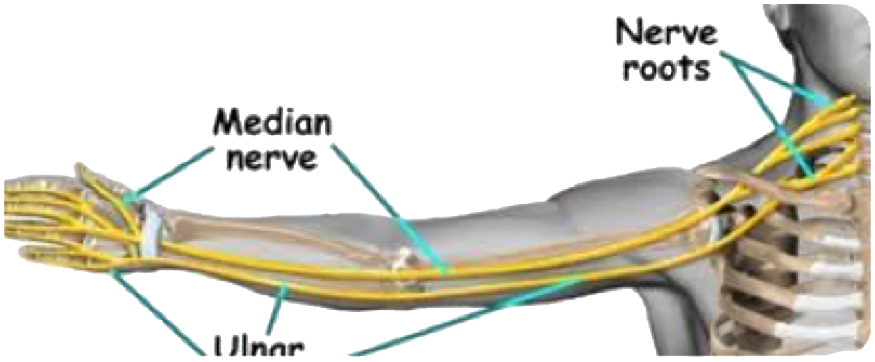
Symptomatic hernias, on the other hand, cause symptoms that depends on the site of nuclear material leakage and hence from the hernia compressed structures, especially the nerve roots.
| Musculoskeletal System: - Arm Pain - Shoulder Blades Pain - Chest Pain - Stiff Neck - Arms and Hands Motor Deficiency - Loss Of Sensitivity - Tingling Urogenital System: - Erection Problems - Urinary incontinence Nervous System: - Dizziness - Drowsiness - Visual Disturbances - Sphincter Control Loss |
 |
Clinical Evaluation:
If the diagnosis is suspected disc herniation, the first required examinations are radiographs and magnetic resonance imaging of the cervical spine. Physical examination can also help in diagnosis, assessing pain, the state of reflexes, sensitivity, strength, and muscle trophism; Based on these diagnoses you can understand which root of the cervical tract is involved.
 |
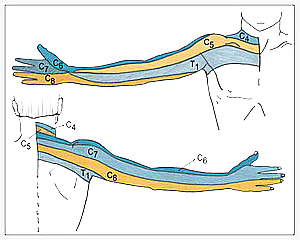 |
| Root Involvement | Location Of Lesion | Referred Pain | Motor Dysfunction | Sensory Dysfunction | Reflex Changes |
| C5 | C4/5 | Shoulder and Upper Arm | Shoulder Muscles (Deltoid-Supraspinatus- Infraspinatus) ↓Abduction and external rotation |
↓Upper and Lateral Aspect of the Shoulder | ↓ Biceps Reflex |
| C6 | C5/6 | Radial Aspect of Forearm | Biceps and Brachialis Muscles ↓Flexion of the Elbow and Supination |
Radial Aspect of Forearm | ↓Thumb Reflex and Brachiradialis Reflex |
| C7 | C6/7 | Dorsal Aspect of Forearm | Triceps Muscle ↓Extension of the Elbow |
↓Index and Middle Digits | ↓ Triceps Reflex |
| C8 | C7/T1 | Ulnar Aspect of Forearm | Intrinsics of the Hand ↓Adduction and Abduction |
↓Ring and Little Digits | No change |
Our Solution:
Percutaneous Mini Invasive Cervical Hernia Laser Treatment.
Discolux® Eutermic Laser: - System for cervical hernias disc decompression at biological temperature.
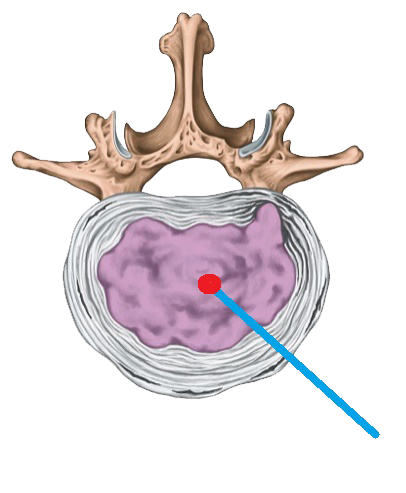 |
With the Discolux® Ho:YAG Euthermic Laser technique, the amount of delivered energy is considerably low, thus obtaining decompression of the intervertebral disc through nucleus gel destruction and colliquation, and not through the vaporization of nuclear gel. This technique allows to maintain the integrity of pulposus nucleus fibroblasts, thus giving the pulposus nucleus the possibility to restore physiologically. |
| The Discolux® Laser Ho: YAG, thanks to its peculiar features, allows to trigger the liquefaction of a nucleus pulpous portion at medium temperatures not exceeding 45 ° C. | 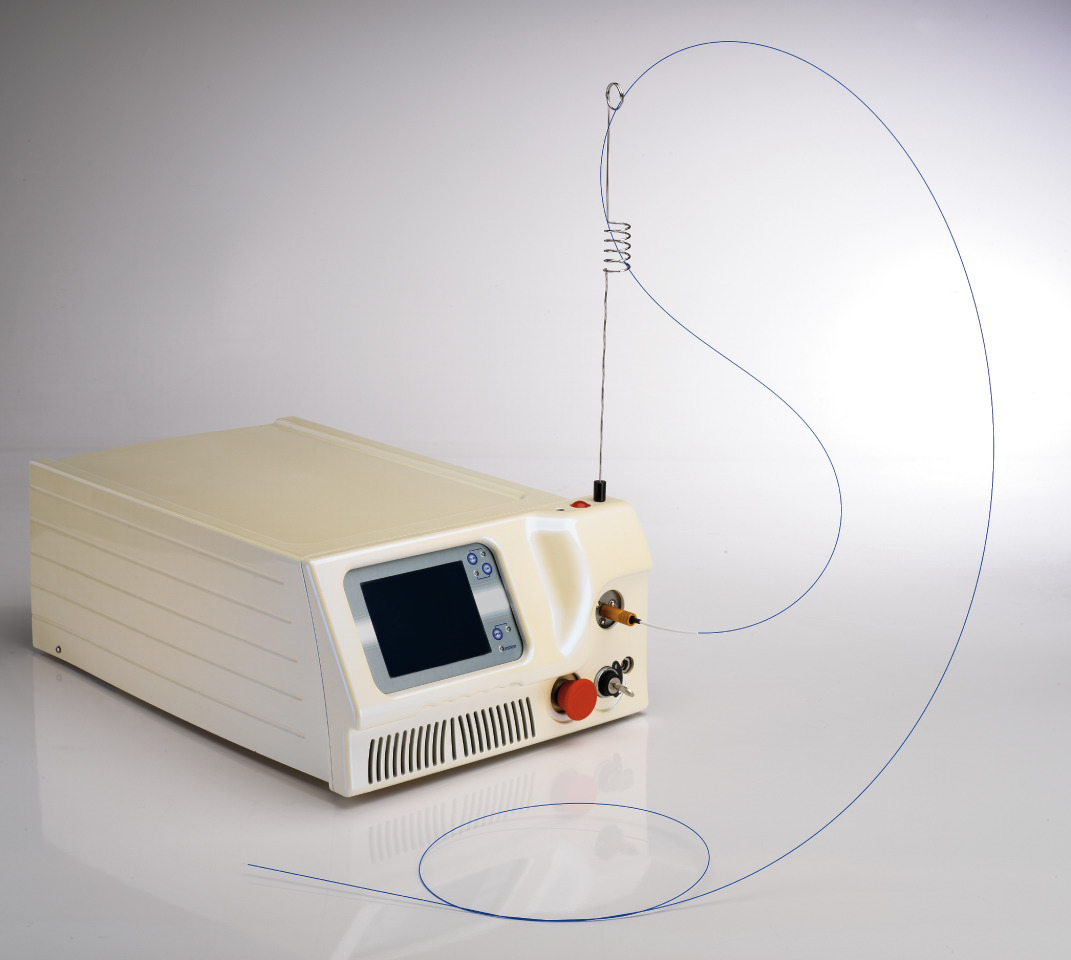 |
How it works:
The Ho:YAG Discolux® Laser therefore involves liquefaction rather than vaporization of the nucleus pulposus, in order to remove part of it to free space and favor resorption of the disk. This makes it possible to perform nucleolysis at much lower temperature (45°C) than the one required for the vaporization of the nucleus (100°C).
Laser Features:
The clinical result is safely and effectively achieved, thanks to the special characteristics of this particular Ho: YAG laser:
- 2100 nm wavelength, for extremely high absorption by water;
- Low energy delivery, to minimize pain for the patient, while treating
and avoid heat build-up, which allows to maintain temperature below 45°C, in the treated area;
- Versatility, to adapt the laser treatment to the actual needs, still maintaining safety and great efficacy.
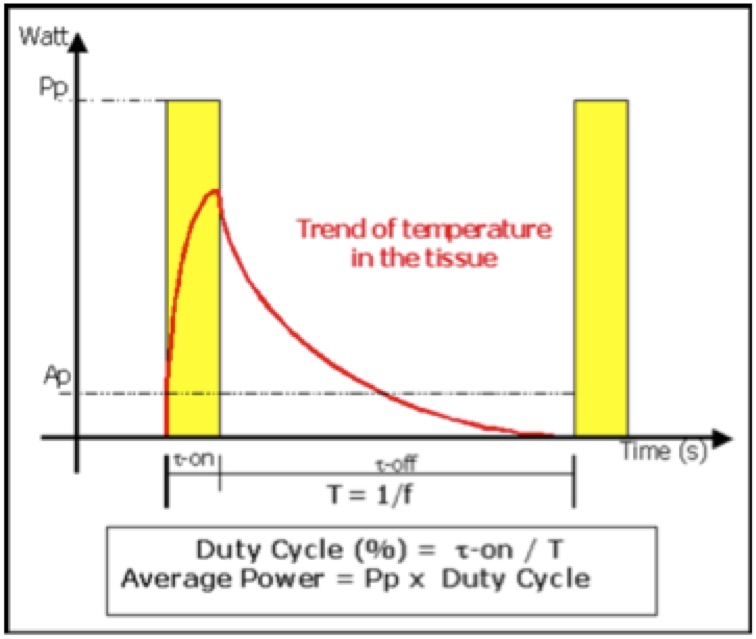
The laser treatment is divided into 3 cyclesof 1 minute each, with 15 second rest time in between cycles.
Exclusive Parameters of Euthermic Ho:YAG 2100nm Discolux® Laser :
Low energy per pulse (150mJ)
Short pulse time (τ-on = 200 μs).
Low frequency (f=10 Hz).
Low total energy (270 J in 3 minutes of total delivered energy).
Very limited thermal growth.
Safety:
The Ho: YAG Discolux® Laser emits a laser beam generated by a Holmium YAG source (Ho:YAG). When delivered into an aqueous medium, said laser beam only penetrates 330 microns from the distal end of the optical fiber. This very minimal penetration of the laser beam, combined with the low energy required for liquefying the nucleus pulposus, limits the thermal action of the laser treatment to an area of few millimeters around the energy emission spot. This technique is therefore adequate for its liquefying action, yet absolutely safe, because it avoids heat build-up in the nucleus pulposus, to the extent that the temperature will never exceed 45°C.
| Thermographies during Euthermic Discolux® Ho: YAG 2100nm Laser emission. 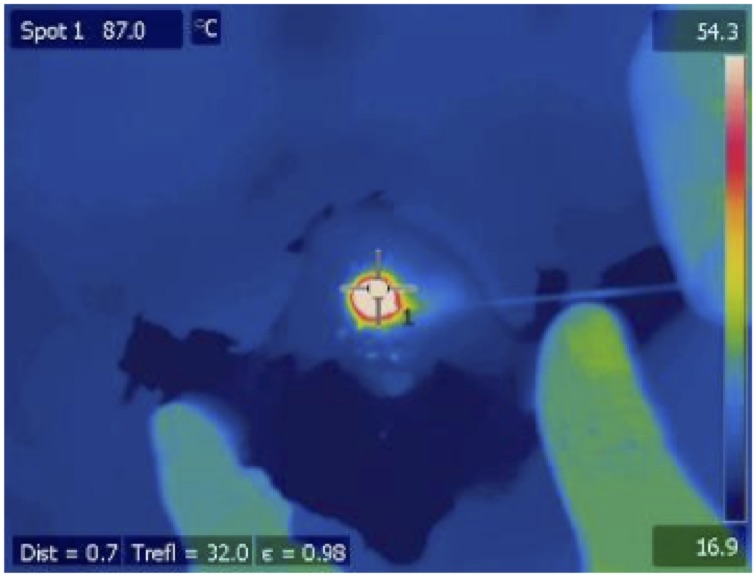 |
Thermographies during 980nm diode laser emission.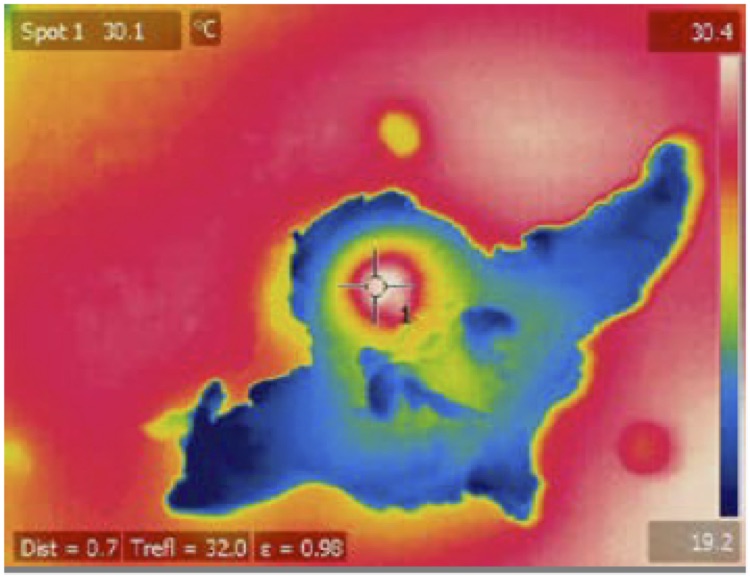 |
This allows to keep the size of the treated area extremely limited, thus avoiding the diffusion of the laser energy to the surrounding tissues and consequently the unwanted increase of temperature off the treated area.
 NESSUN RISCHIO DI DANNO TERMICO. |
The picture shows the pulse cycle of the Discolux® laser. It is very important to note the length of inactivity time between a pulse and the following; this is a key feature to control temperature accumulation. Low frequencies (long intervals) or low pulse energies, are effective means to control the thermal impact. In this way, excessive buildup of heat can be avoided before causing structural damage to the surrounding tissues. NO RISK OF THERMAL DAMAGE.
|
Pros:
• Biological Temperature
• Percutaneous technique
• Checks on removed material
• Safe
• Fast
• No risk of thermal damage
• Immediate wellness for the patient
Indications:
Percutaneous disc decompression using Discolux® laser system, is indicated in patients with a low degree of protrusion of grade I and II in the cervical tract discs.
 |
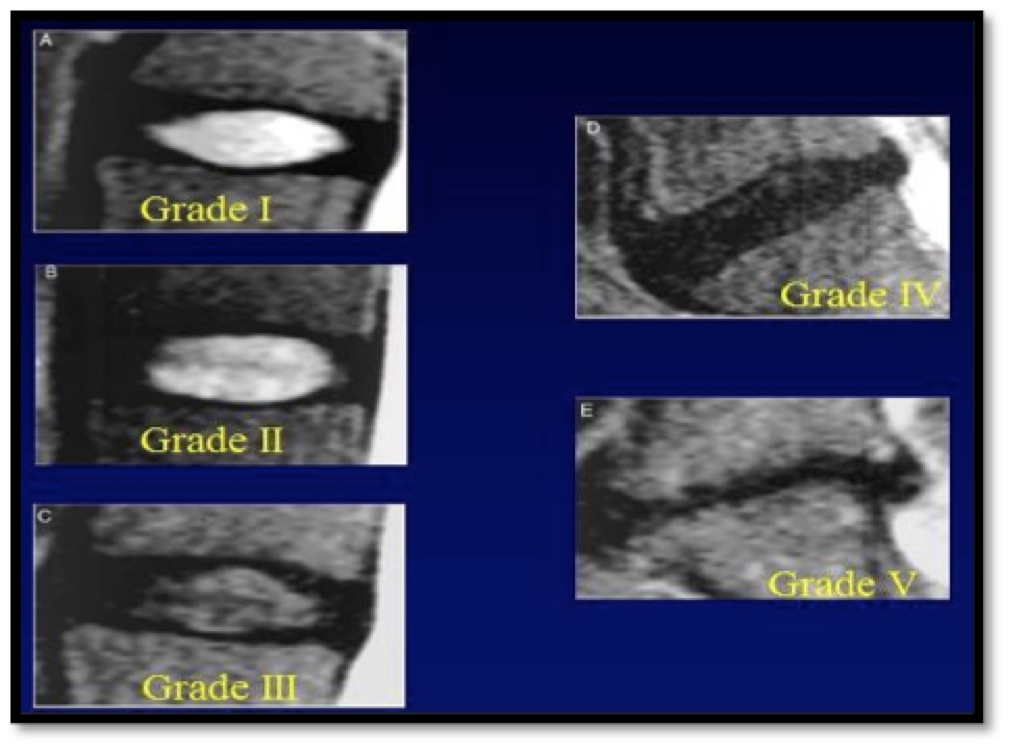 |
Contraindications:
Absolute contraindications preventing the use of the Discolux® - Cervical are:
- The instrument is not suitable to treat patients with presence of column damages, infections, tumors, severe infirmity, status of pregnancy.
- The instrument is not suitable to treat patients with bone fragments, severe bone stenosis.
- The instrument is not suitable to treat patients with severe neurological deficit.
Other relative contraindications are:
- non collaborating patient, patient unable to follow operator’s instructions;
- osteomalacia;
- non local infection potentially interesting the treated regions;
- hypotension;
- congestive hearth disease;
- renal failure.
Discolux® - Cervical Kit:
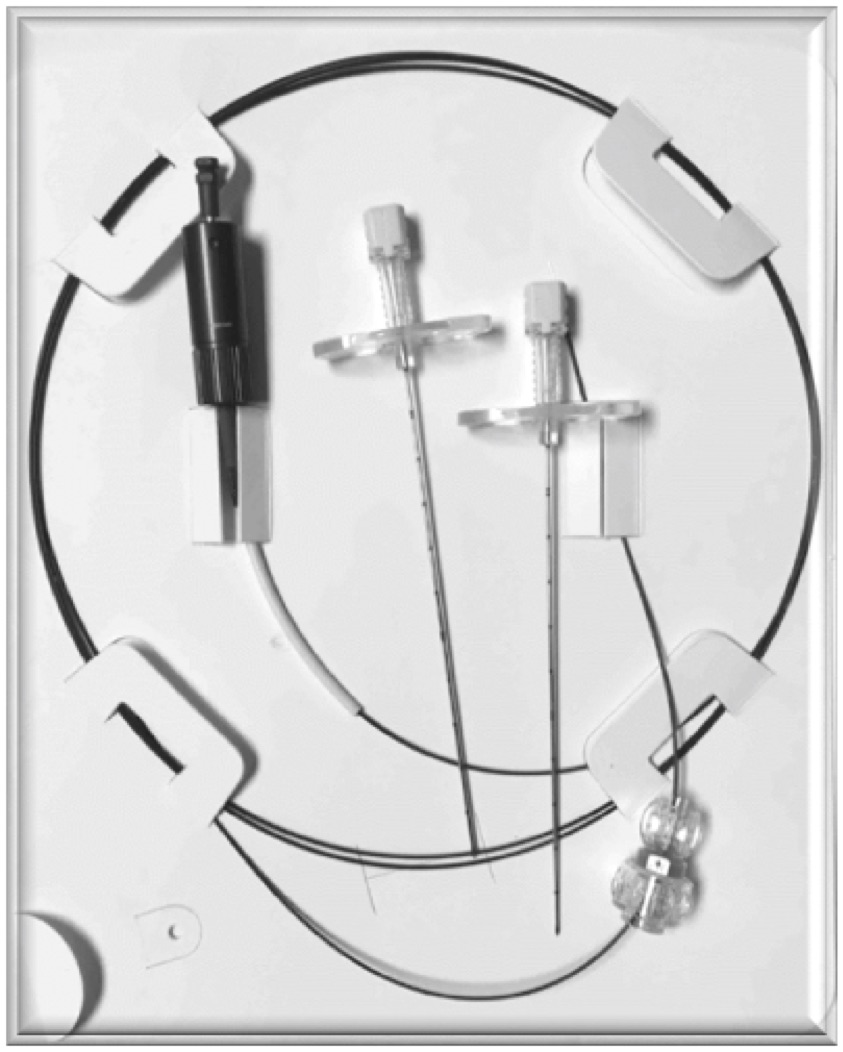 |
The Discolux® laser system is equipped with a sterile and disposable access kit, made up of: • 1 optical fiber to connect to the Discolux® laser, only. • 2 needles for vertebral access - 20 G size - 11 cm long (Code: CBL20 / 11) • 1 fiber block to fix the distal part of the optical fiber to the access needle. |
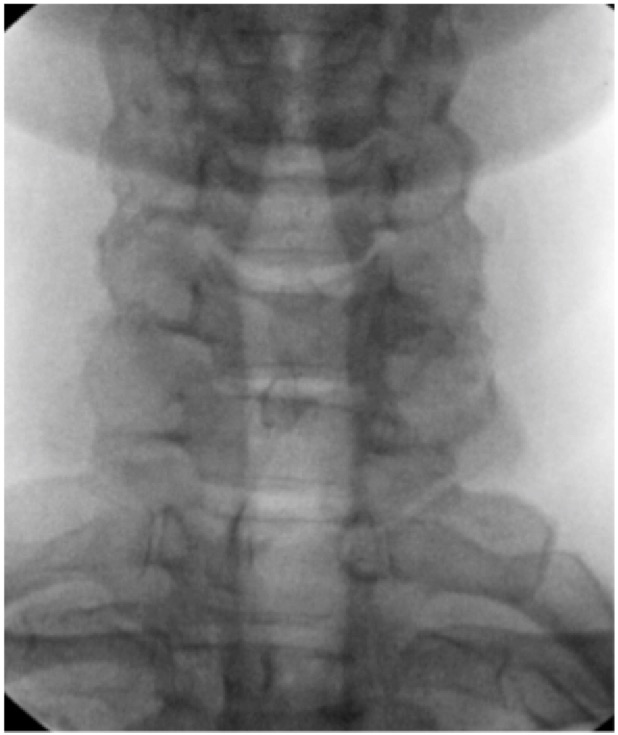
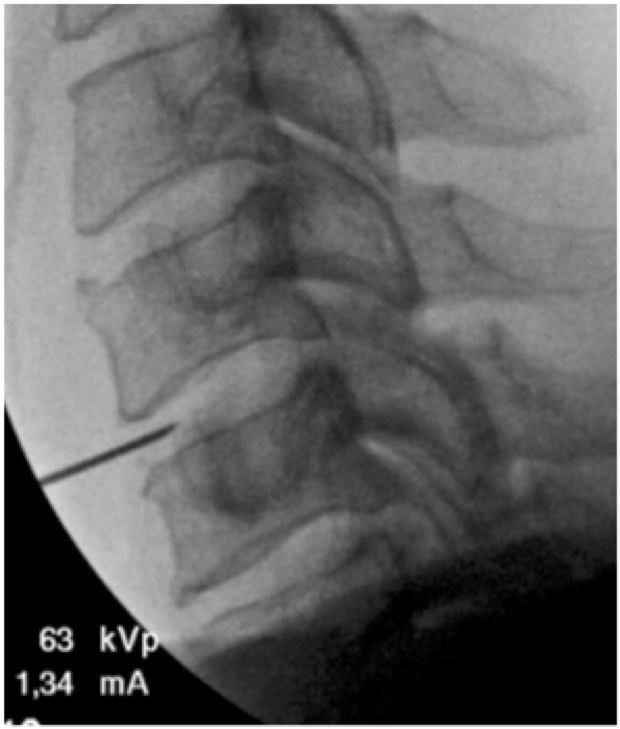
Operating Technique:
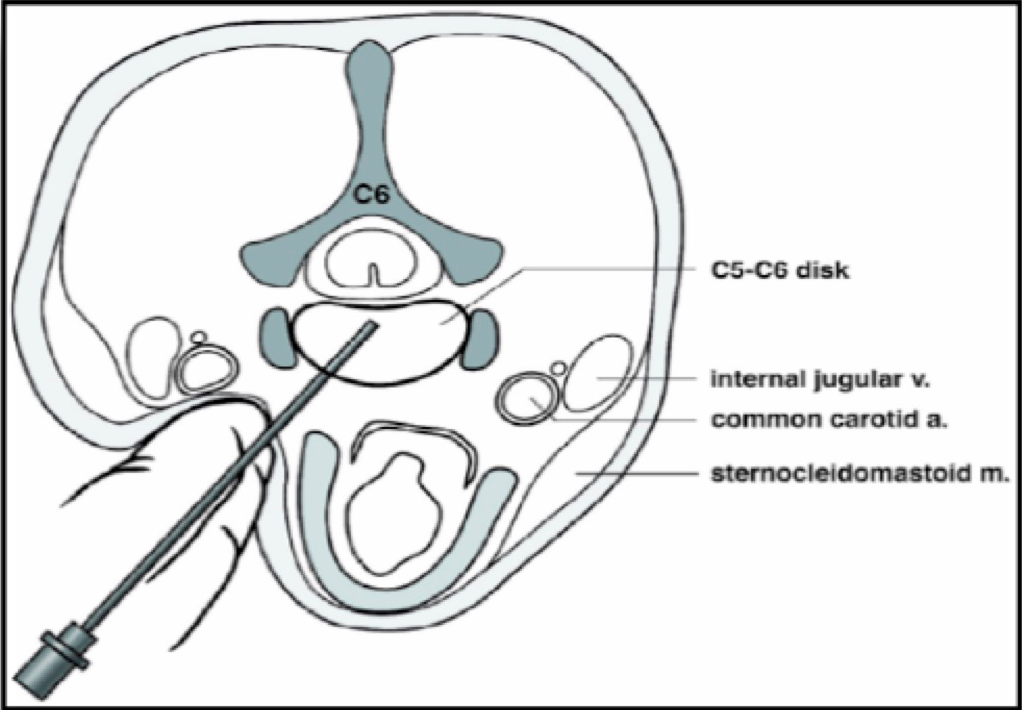 |
With the supine patient, once located the disc to be treated, access frontally to the pulposus nucleus through the CBL 20/11 insert needle. |
 |
 |
 |
 |
 |
 |
Once the appropriate point is reached inside the disc, insert the optical fiber into the needle and connect it to the Discolux® laser system.
Laser Treatment::
Connect the fiber to the laser; The entire procedure is handled by the software of the Discolux® unit and its duration is 3.45 minutes total, divided into 3 phases:
Each phase consists of 1 minute (60 Seconds) continuous laser output with a power of 1.5 W, followed by 15 seconds of rest.
| PHASE 1 | PHASE 2 | PHASE 3 | |||
| ENERGY | REST | ENERGY | REST | ENERGY | REST |
| 60 sec. | 15 sec. | 60 sec. | 15 sec. | 60 sec. | 15 sec. |
The total energy delivered will be 270 J in 3 minutes, reaching the REDUCTION OF INTRADISCAL PRESSURE.
Immediate Wellness:
| At the end of the 4-minute Discolux laser treatment, the patient will be immediately relieved of the pain and, thanks to minimal invasiveness of the intervention, will find a feeling of instantaneous well-being. |  |
Certifications:
CE Discolux Laser |
CE Discolux Kit |
Bibliografy:
[1] Boswell MV, Trescot AM et al. Interventional techniques: evidence-based practical guidelines in the management of chronic spinal pain. Pain Physician 2007; 10:7-111.
[2] Gibby W. Automated percutaneous discectomy. In: Handbook of diagnostic and therapeutic spine procedures. A.L. Williams and F.R. Murtagh, Editors. St Louis: CV Mosby, 2002: 203-225.
[3]. Fenton DS, Czervionke LF. Discography. In: Handbook of diagnostic and therapeutic spine procedures. A.L. Williams and F.R. Murtagh, Editors. St Louis: CV Mosby, 2002: 167-199.
[4]. Fraser RD, Osti OL, Vernon-Roberts B. Discitis after discography. J Bone Joint Surg Br 1987; 69: 31.
[5]. Zeidman SM, Thompson K, Ducker TB. Complications of cervical discography: Analysis of 4400 diagnostic disc injections. Neurosurgery; 37: 414.
[6]. Simopoulos TT, Kraemer JJ, Glazer P, Bajwa ZH. Vertebral osteomyelitis: a potentially catastrophic outcome after lumbar epidural steroid injection. Pain Physician 2008 Sep-Oct; 11(5): 693-7.
[7] Smuck M, Benny B, Han A, Levin J. Epidural fibrosis following percutaneous disc decompression with coblation technology. Pain Physician. 2007 Sep; 10(5):691-6.
[8] Appleby D, Andersson G, Totta M. Metaanalysis of the efficacy and safety of intradiscal electrothermal therapy (IDET). Pain Med 2006; 4: 308-316.
[9] Gangi A, Dietemann JL, Ide C, Brunner P, Klinkert A, Warter JM. Percutaneous laser disc decompression under CT and fluoroscopic guidance: Indications, technique and clinical experience. Radiographics 1996; 16: 89-96.
[10] Connor PM, Darven BV. Cervical discography complications and clinical efficacy. Spine 1993; 18(14): 2035.
[11] Bogner EA. Past, present and future of therapeutic lumbar spine interventional procedures. Radiol Clin N Am 2009; 47(3): 411-419.
[12] Gangi A, Dietemann JL, Ide C, Brunner P, Klinkert A, Warter JM. Percutaneous laser disc decompression under CT and fluoroscopic guidance: Indications, technique and clinical experience. Radiographics 1996; 16: 89-96.
[13] Fenton DS, Czervionke LF. Intradiscal electrothermal therapy. In: Image guided spine intervention. Saunders 2003; 257-285.
[14] Fenton DS, Czervionke LF. Discography. In: Handbook of diagnostic and therapeutic spine procedures. A.L. Williams and F.R. Murtagh, Editors. St Louis: CV Mosby, 2002: 167-199.
[15] Eckel, TS. Intradiscal electrothermal therapy. In: Handbook of diagnostic and therapeutic spine procedures. A.L. Williams and F.R. Murtagh, Editors. St Louis: CV Mosby, 2002: 229-244.