DISCOLUX LUMBAR PLDD: Percutaneous Mini Invasive Lumbar Hernia Laser Decompression.
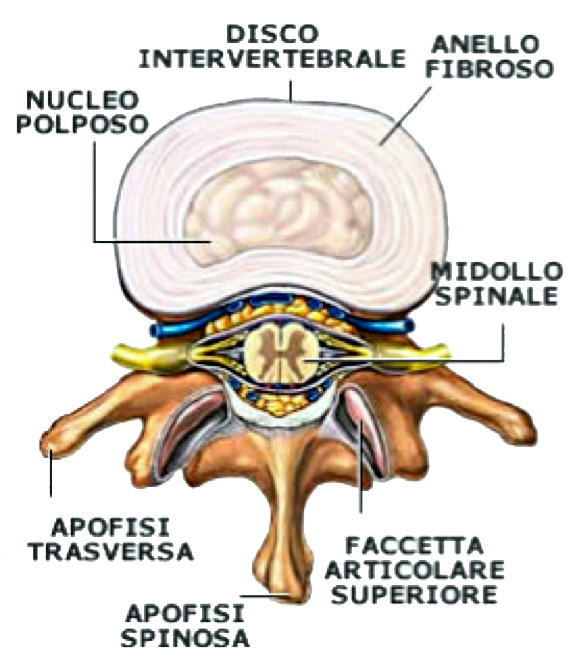
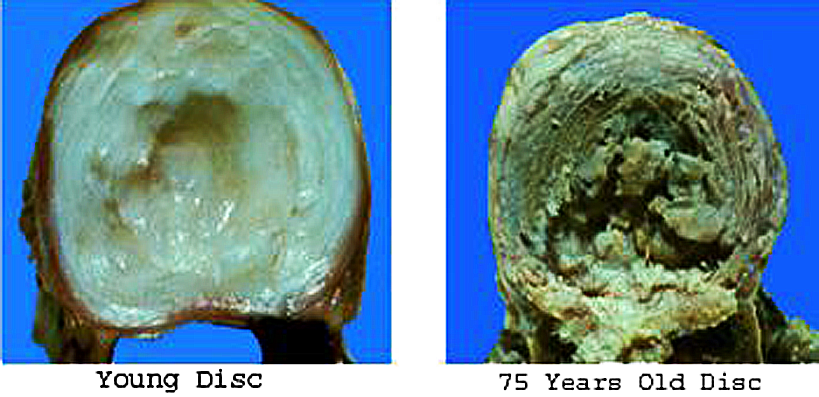
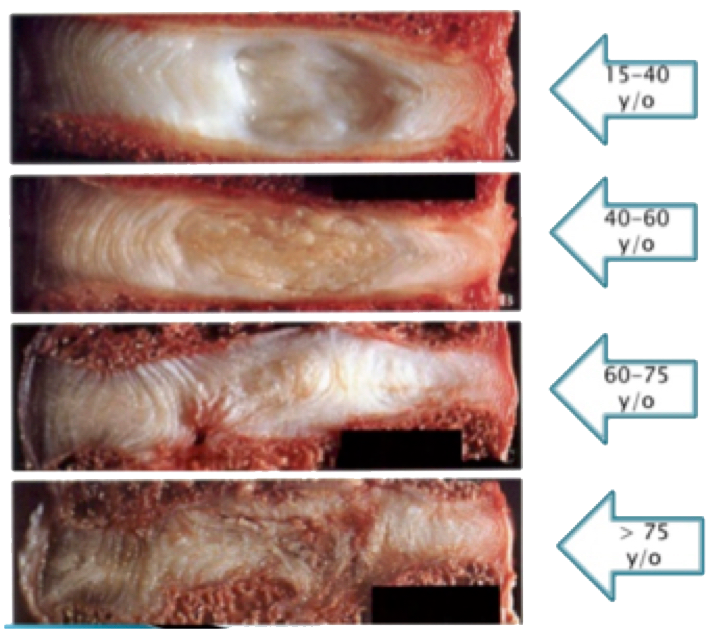
Description:The disc hernia is a spine desease consisting of a rupture or dislocation of disc's fibrous ring, and subsequent dislocation of the polpous nucleus.Disc rupture and / or bulging are generally secondary to a degeneration or aging, a phenomenon that starts with disc cartilages. Degeneration and therefore disk hernia are often linked to genetic-family congenital factors, activated or revealed by various causes such as stress and vertebral trauma, protracted spoiled postures, maldistribution of loads on the column and others. |
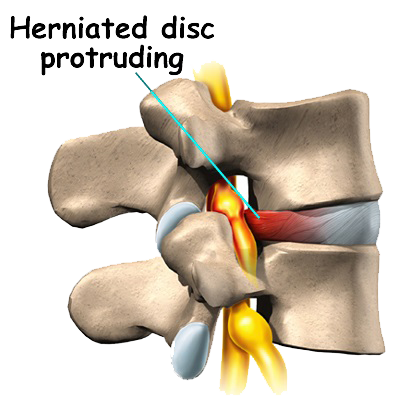 |
The most common hernias are the lumbar, followed by the cervical and dorsal ones; frequent cases of multiple hernias. All ages can be affected by disc hernia.
|
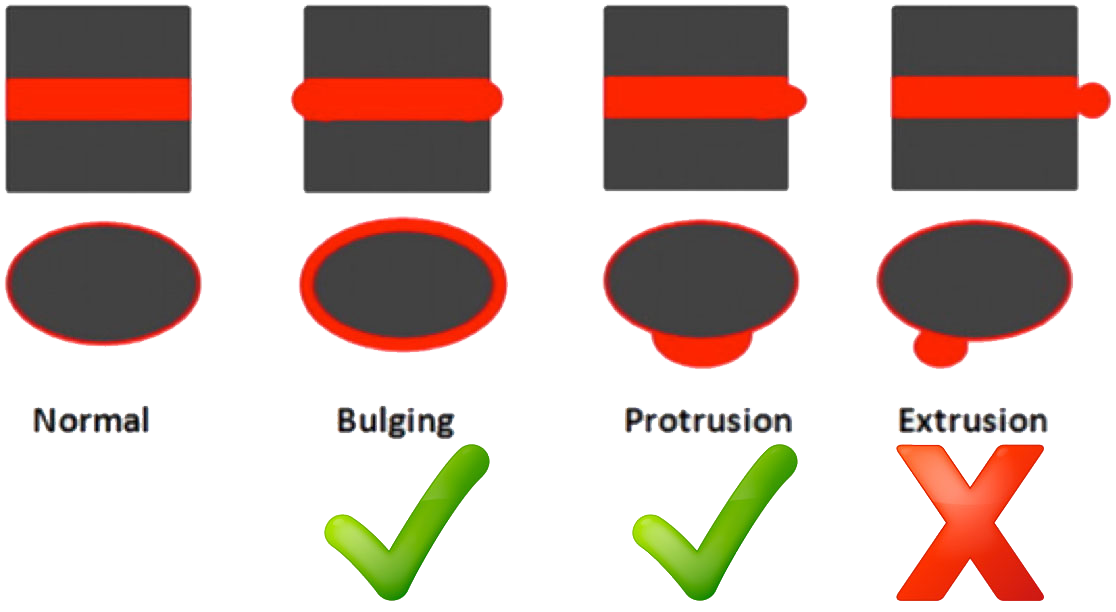
The herniated disc differs depending on where it is located:
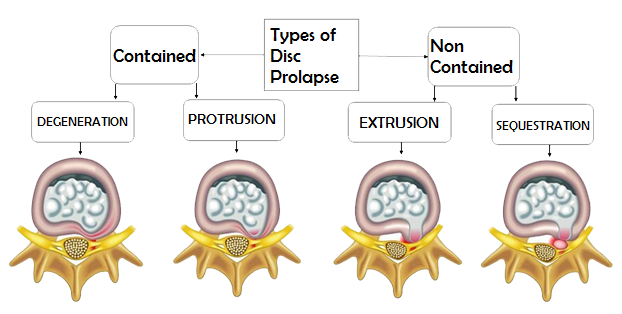
• central, the most frequent; • posterolateral; • foraminal; • extraforaminal, the rarest; • subligamentous; • transligamentous. Hernia can also be classified according to the fibrous annulus conditions, the ring surrounding the nucleus: Contained Hernia (Intact annular fibres): - Disc degeneration: The disc appears swollen, but the annular fibers and the longitudinal rear ligament appear intact. - Disc Protrusion: Internal annular fiber breaks, but the outer annular fibers remain intact. Non Contained Hernia (Disruption of annular fibres): - Disc Extrusion: Annulus rupture with tail material that extends into the disk space. - Disc Sequestration: When the ring break and the inner discal fluid leaks in the vertebral channel. |
 |
Risk factors:
In addition to wear caused by aging, other factors may increase the disc hernia likelihood:
• Irregular posture of the back. Using back muscles to lift heavy objects without bending your knees can cause a disk hernia for the strong pressure exerted on the intervertebral discs.
• Gender. Men between the ages of 30 and 50 are more likely to have a hernia.
• Weight. Being overweight adds tension on the back disks.
• Repetitive activities that strain the spine.
• Many jobs are physically weary, some foreseeing continuous lifting, pulling, flexing or twisting.
• Driving for long periods. Vibrations put pressure on the spine and discs.
• Sedentary lifestyle. Regular exercise is important in preventing many diseases, including a disc hernia.
• Smoking. Smoking cigarette is believed to reduce oxygen supply to the disc and cause faster degeneration.
• Cervical hernia may be caused by road accidents that cause whiplash or other trauma.
 |
 |
Symptoms:
Many hernias are asymptomatic.
In the symptomatic ones there are vertebral, cervical, dorsal or lumbar pain, depending on the site of the hernia and possible compression disorders of the nerve structures (spinal cord and roots) that are in the vertebral canal.
Some possible symptoms of lumbar hernia:
• Lumbar pain.
• Lumbar radiculopathy or sciatica (dolore alla gamba o al piede).
• Lumbar cruralgia.
• Feelings of sensitivity, motility, trophism, and reflexes in the lower limbs.
• Difficult to stand still for a long time.
• Weakness in the legs or feet.
• Sexual disorders.
• Sphincter disorders.
Our Solution:
Euthermic Discolux® Laser - Lumbar disc herniated decompression System at biological temperature.
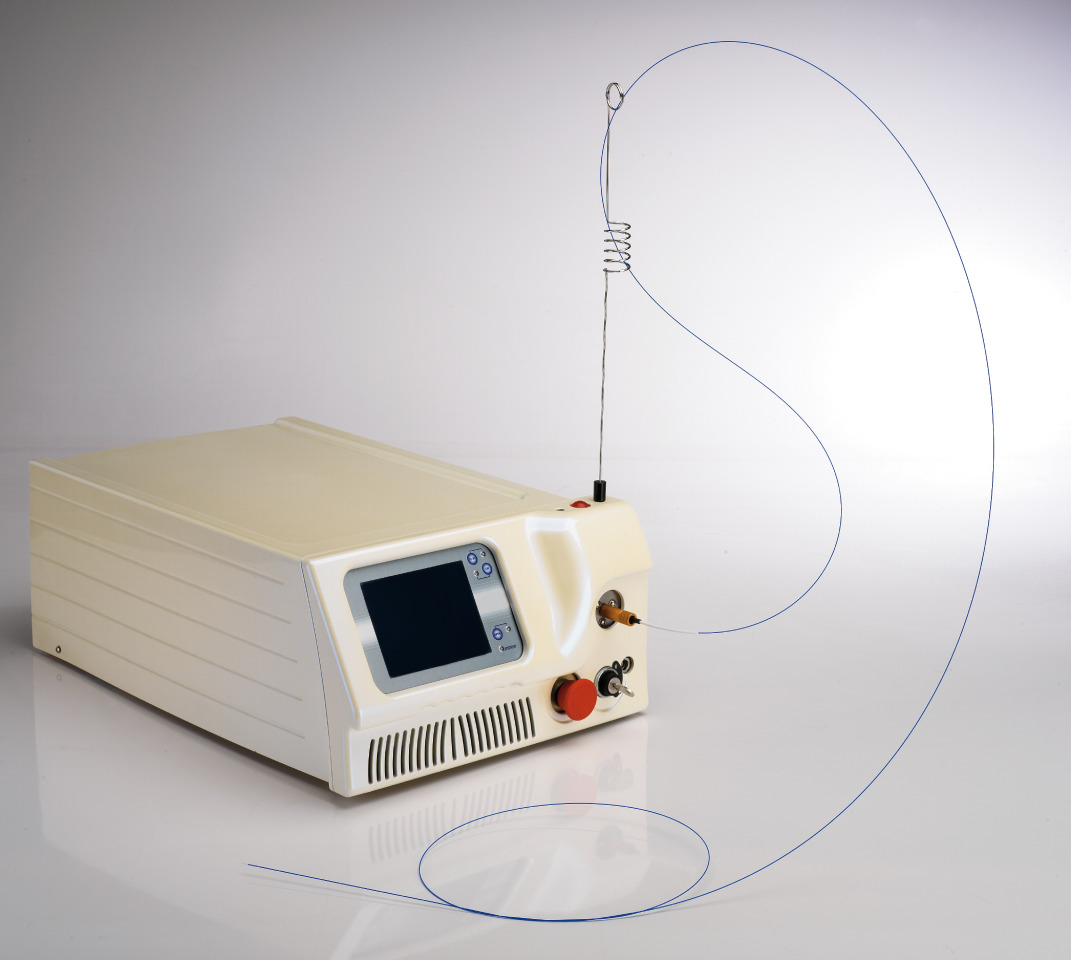 |
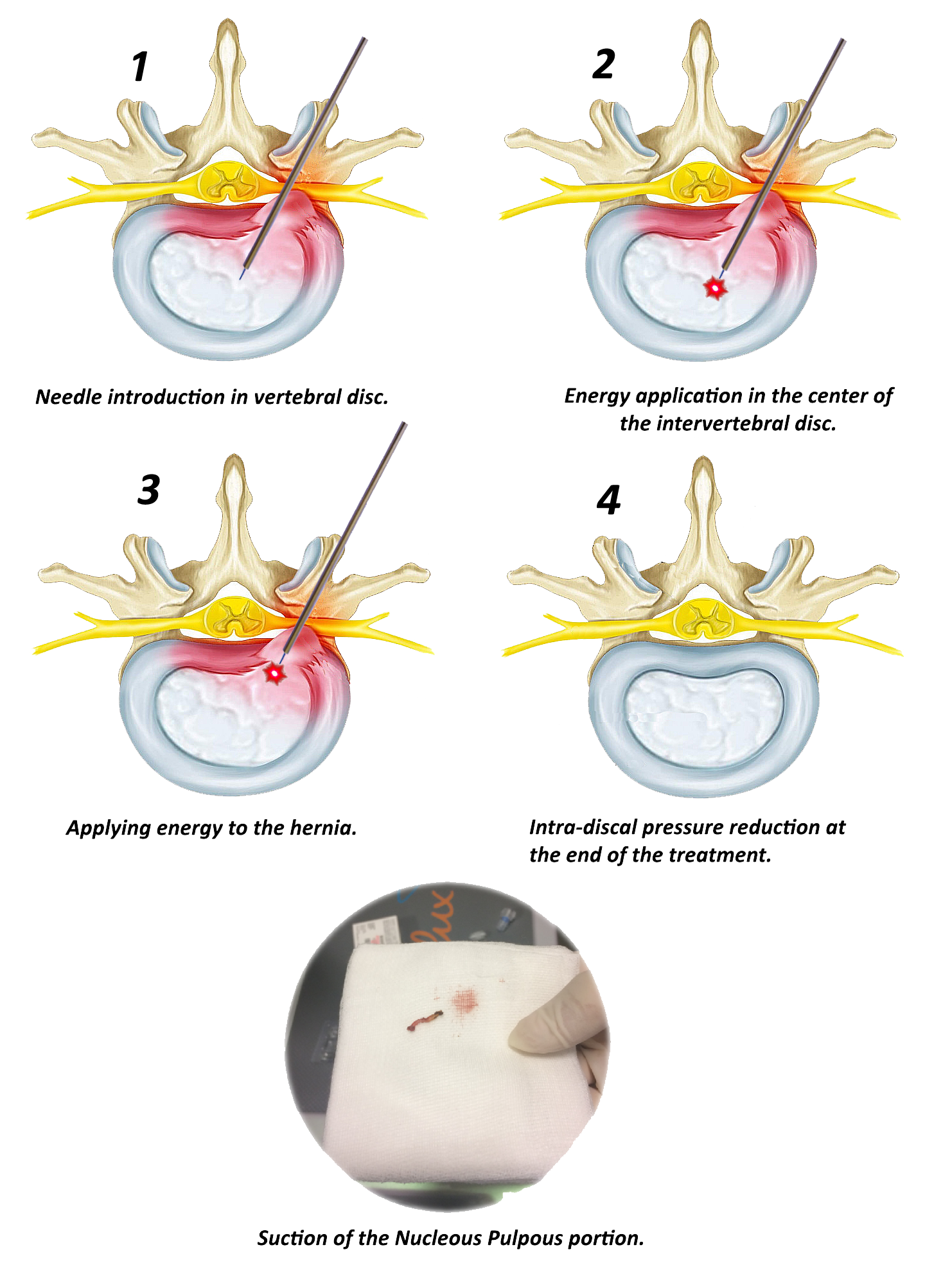
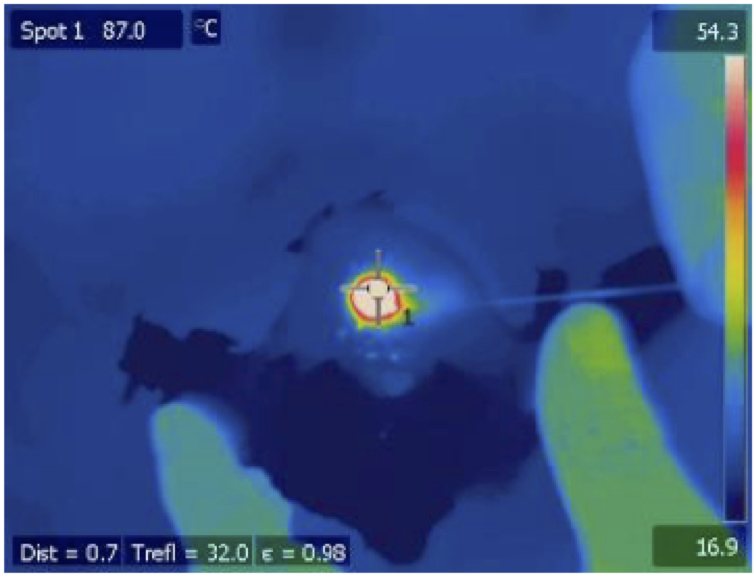
This assisted laser disc decompression technique involves the suction of a nucleus pulpous portion, which is liquefied at a very low temperature in order to reduce the internal pressure of the pathological disk, without compromising the viability of residual fibroblasts. The Discolux® Laser Ho: YAG, thanks to its peculiar features, allows to trigger the liquefaction of a nucleus pulpous portion at medium temperatures not exceeding 45 ° C. |
How It Works:
The Ho:YAG Discolux® Laser therefore involves destructuring rather than vaporizing the nucleus pulposus, in order to allow to suck out part of it, by means of applying a negative pressure. This makes it possible to perform nucleolysis at much lower temperature (45°C) than the one required for the vaporization of the nucleus (100°C).
Laser Features:
Exclusive Features of Euthermic Ho:YAG 2100nm Discolux® Laser :
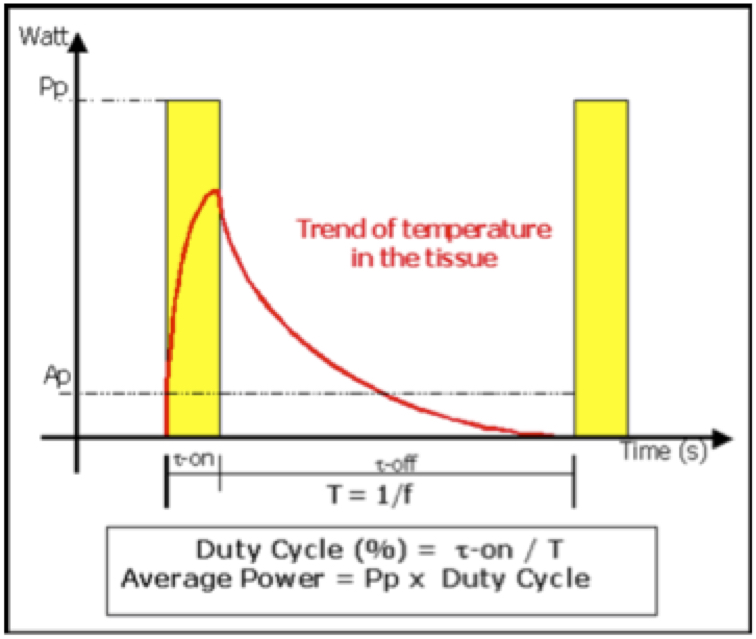
Low energy per pulse (300mJ)
Short pulse time (τ-on = 200 μs).
Low frequency (f=7 Hz).
Low total energy (756 J in 6 minutes of energy delivery).
Very limited thermal growth.
Safety:
The Ho: YAG Discolux® Laser emits a laser beam generated by a Holmium YAG source (Ho:YAG). When delivered into an aqueous medium, said laser beam only penetrates 330 microns from the distal end of the optical fiber. This very minimal penetration of the laser beam, combined with the low energy required for liquefying the nucleus pulposus, limits the thermal action of the laser treatment to an area of few millimeters around the energy emission spot. This technique is therefore adequate for its liquefying action, yet absolutely safe, because it avoids heat build-up in the nucleus pulposus, to the extent that the temperature will never exceed 45°C.
| Thermographies during Euthermic Discolux® Ho: YAG 2100nm Laser emission. |
Thermographies during 980nm diode laser emission. |
|
 |
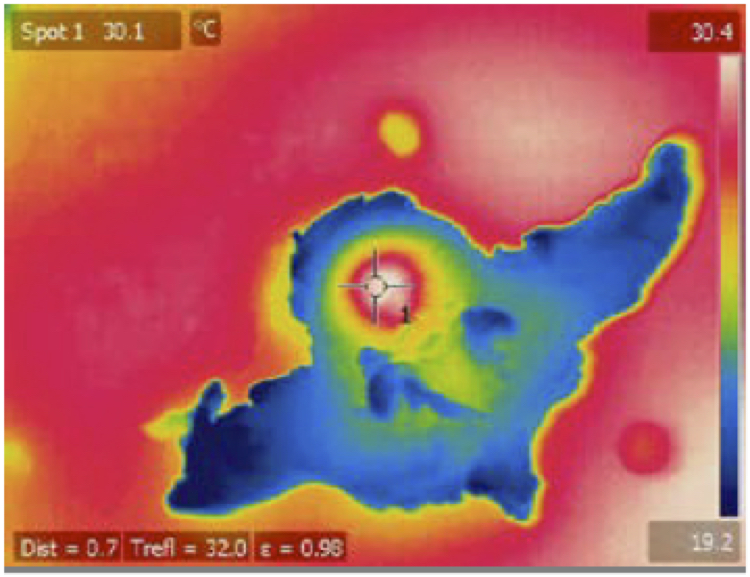 |
The penetration coefficient in water of Ho: YAG Discolux® Laser, limits the penetration in of the laser beam into water-rich (soft) tissues is 0,33 mm from the distal end of the fiber, in comparison to the 20 mm penetration of standard diodic lasers (980 nm).
This allows to keep the size of the treated area extremely limited, thus avoiding the diffusion of the laser energy to the surrounding tissues and consequently the unwanted increase of temperature off the treated area.
|
NESSUN RISCHIO DI DANNO TERMICO. |
The picture shows the pulse cycle of the Discolux® laser.
NO RISK OF THERMAL DAMAGE. |
Pros:
• Biological Temperature
• Percutaneous technique
• Checks on removed material
• Safe
• Fast
• No risk of thermal damage
Indications:
The success of the procedure depends largely on the selection of the lesions to be treated: disc hernia must be at least partially contained by the outer disc fibers, without extensive extrusion, sequestration, or fragment migration.
• Lumbar sciatica /Lumbar cruralgia
• Recurrent drug-resistant symptoms with no or minimum pain reduction after 4-6 weeks of conservative therapy
• RM positive at the same metameric level of clinically evaluated symptoms
• Contained or extruded disc hernias, without free fragments (ASNR classification) and Pfirrmann disc degeneration grade I-III (sufficient hydration of the disc)
• Disc height >50% physiological height
• Small / medium sized protrusions.
Contraindications:
• Expelled hernias
• "Free" disc fragments
• Disc or vertebral body infections
• Cauda equina syndrome
• Disabling motor deficit
• Calcified hernias
• Big sized hernias
• Spinal stenosis
• Failed back surgery syndrome (FBSS)
Discolux® Kit:
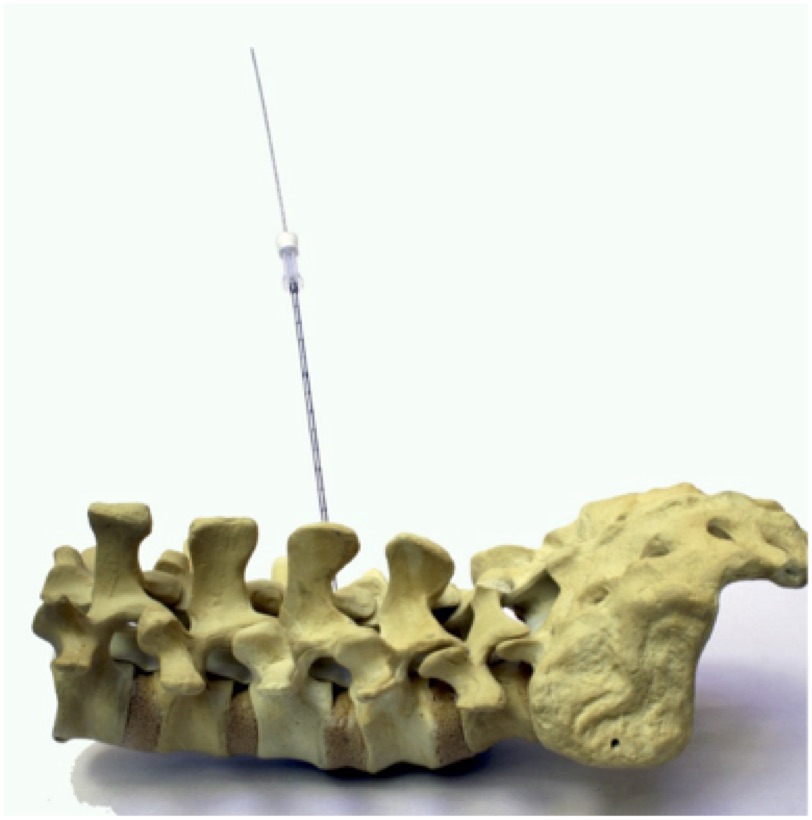
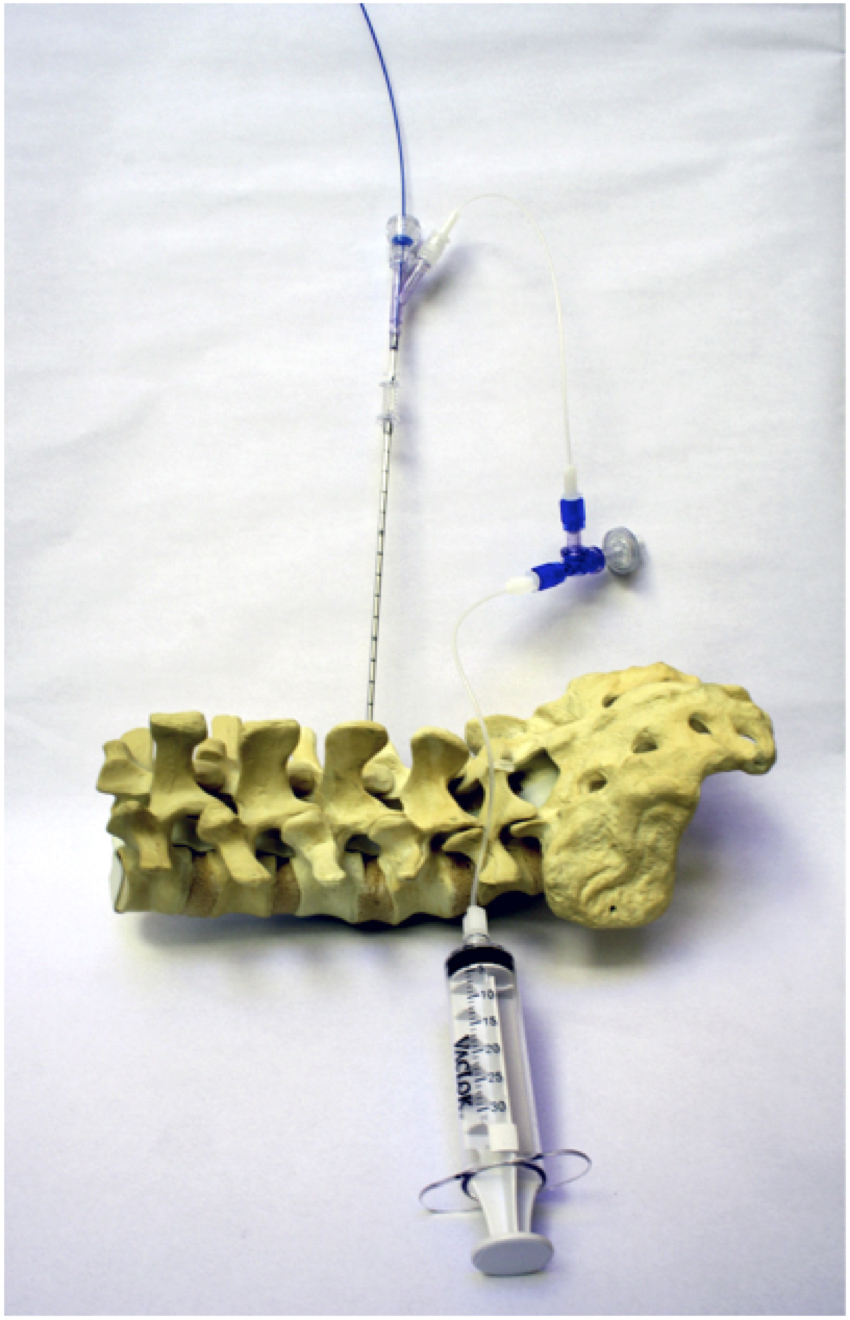
Discolux® Euthermic Disc Decompression (PLDD) is a percutaneous technique that can be performed with a dedicated Procedural Kit.
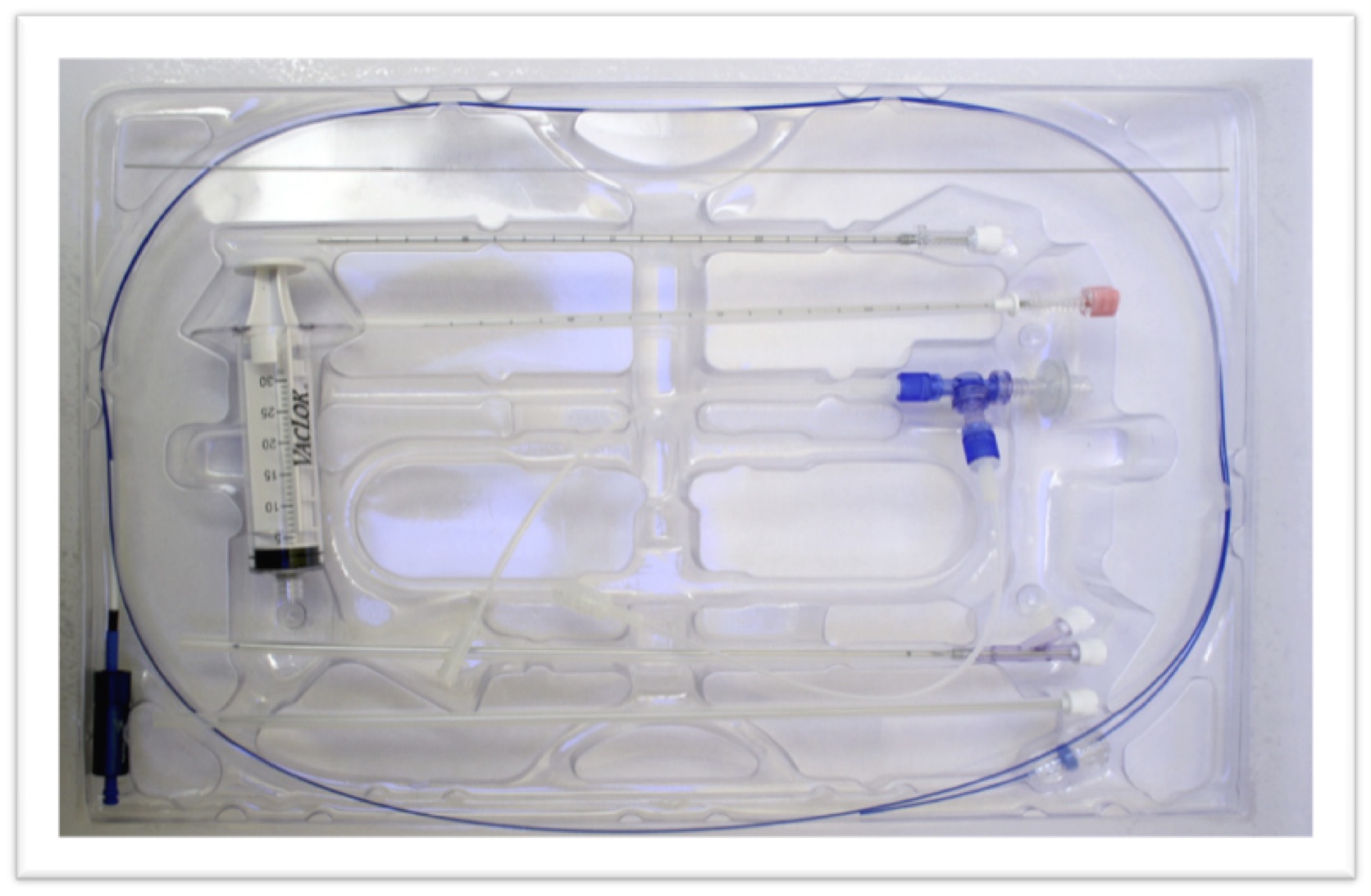
| Code | Description | |
| CBL 18/20 | Chiba needle for anesthesia and first access. |  |
| RK0518/38 | Guidewire |  |
| DBC13/19 | Trocar cannula to the intervertebral disc | 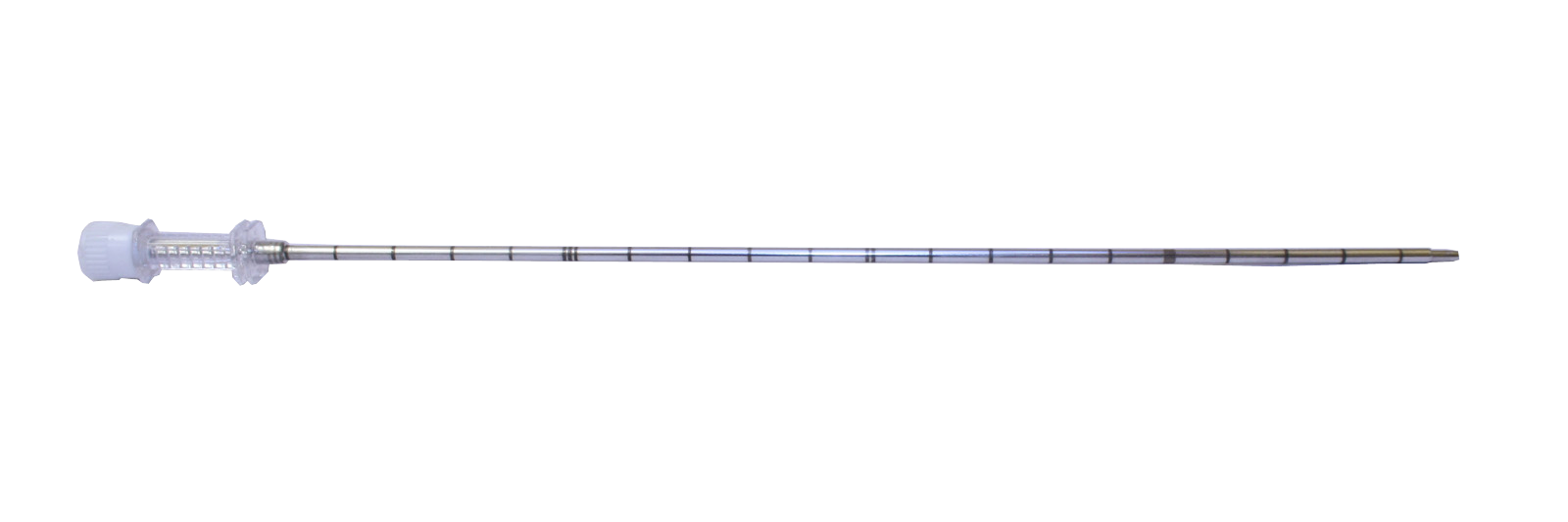 |
| DCL14/20 | Working cannula | 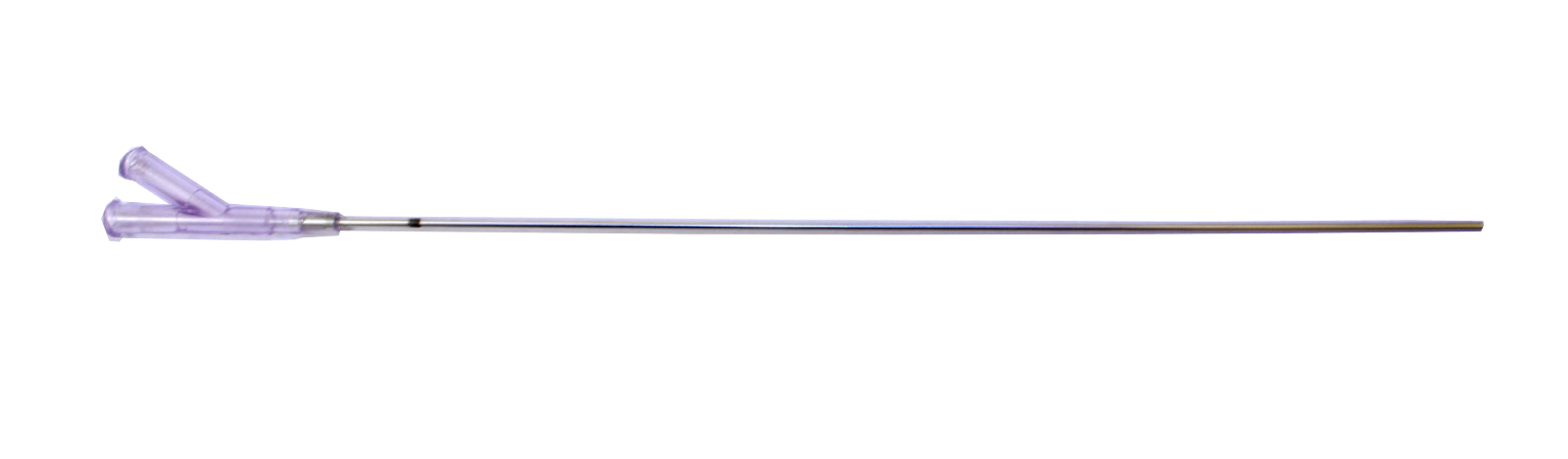 |
| VS30 CT40 | System for connection and vacuum aspiration | 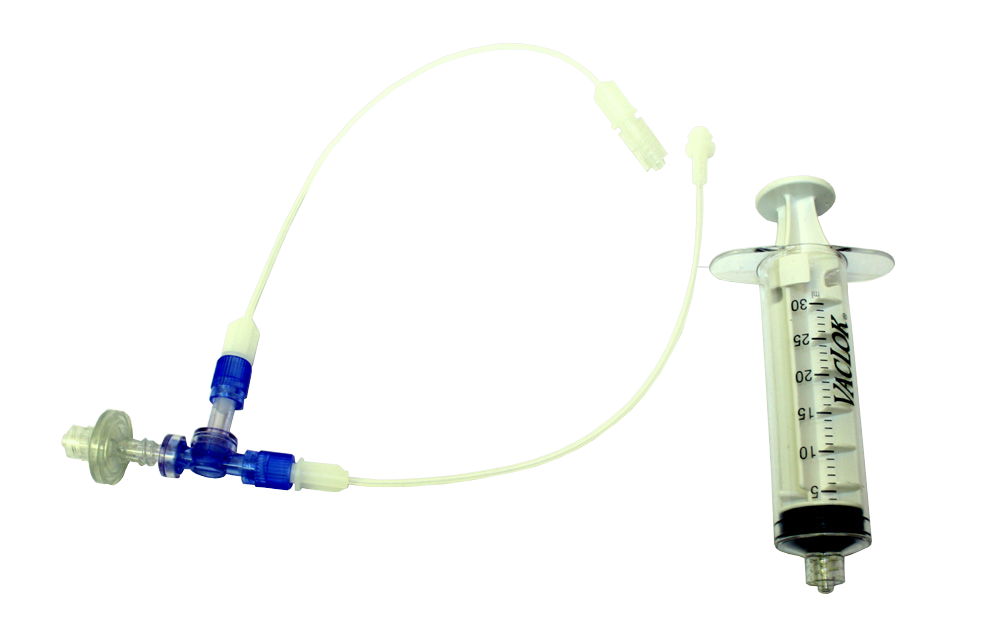 |
| FBR08225 | Discolux® Optical Fiber with fiber-lock connector | 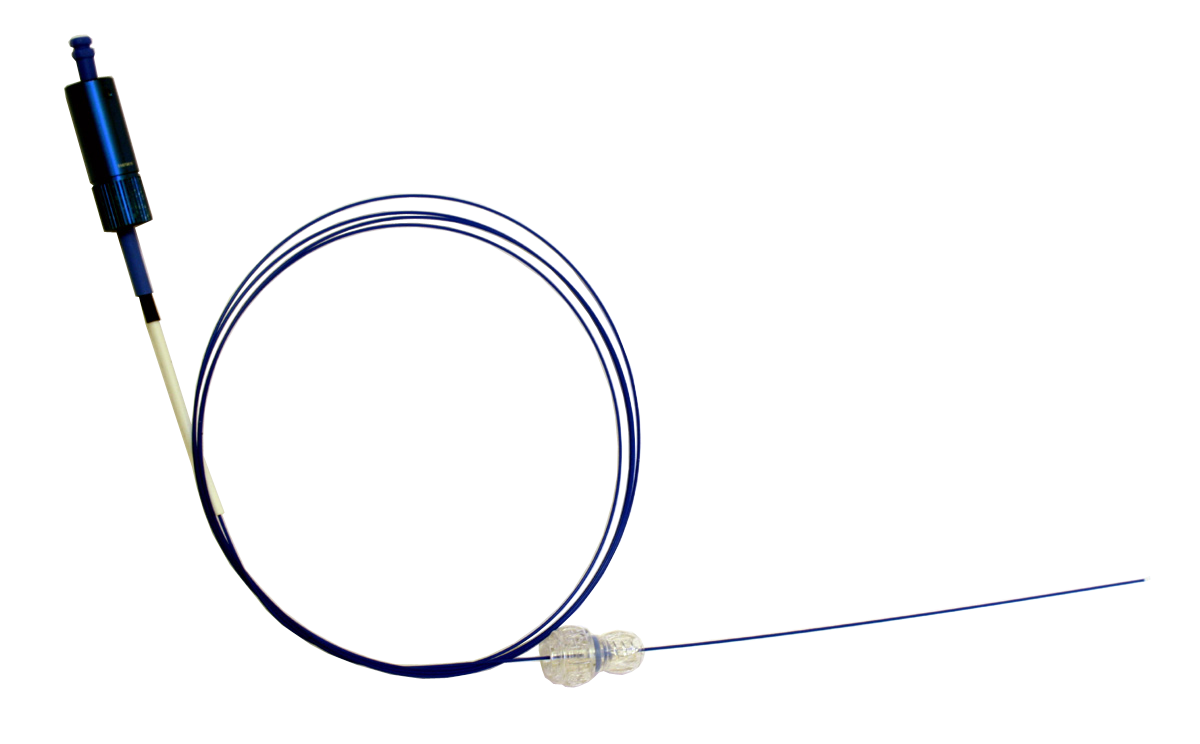 |
Operating Technique:
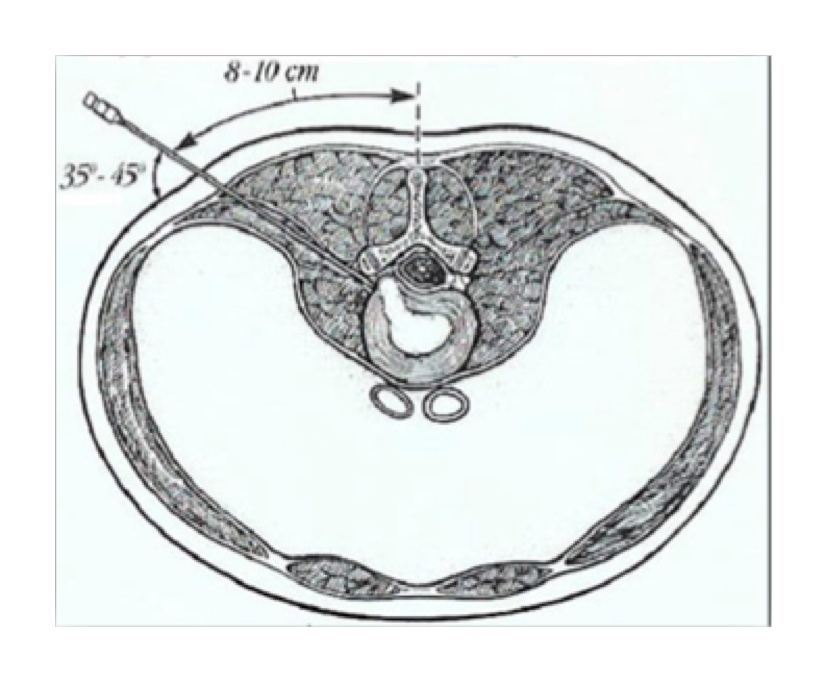
The patient is placed prone with suitable supports to improve the position for access to the disc and to protect blood vessels and nerves from compression.
 |
 |
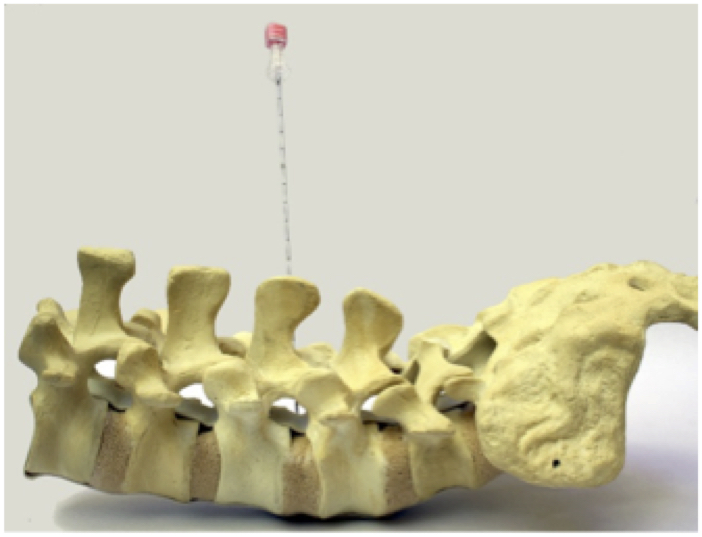
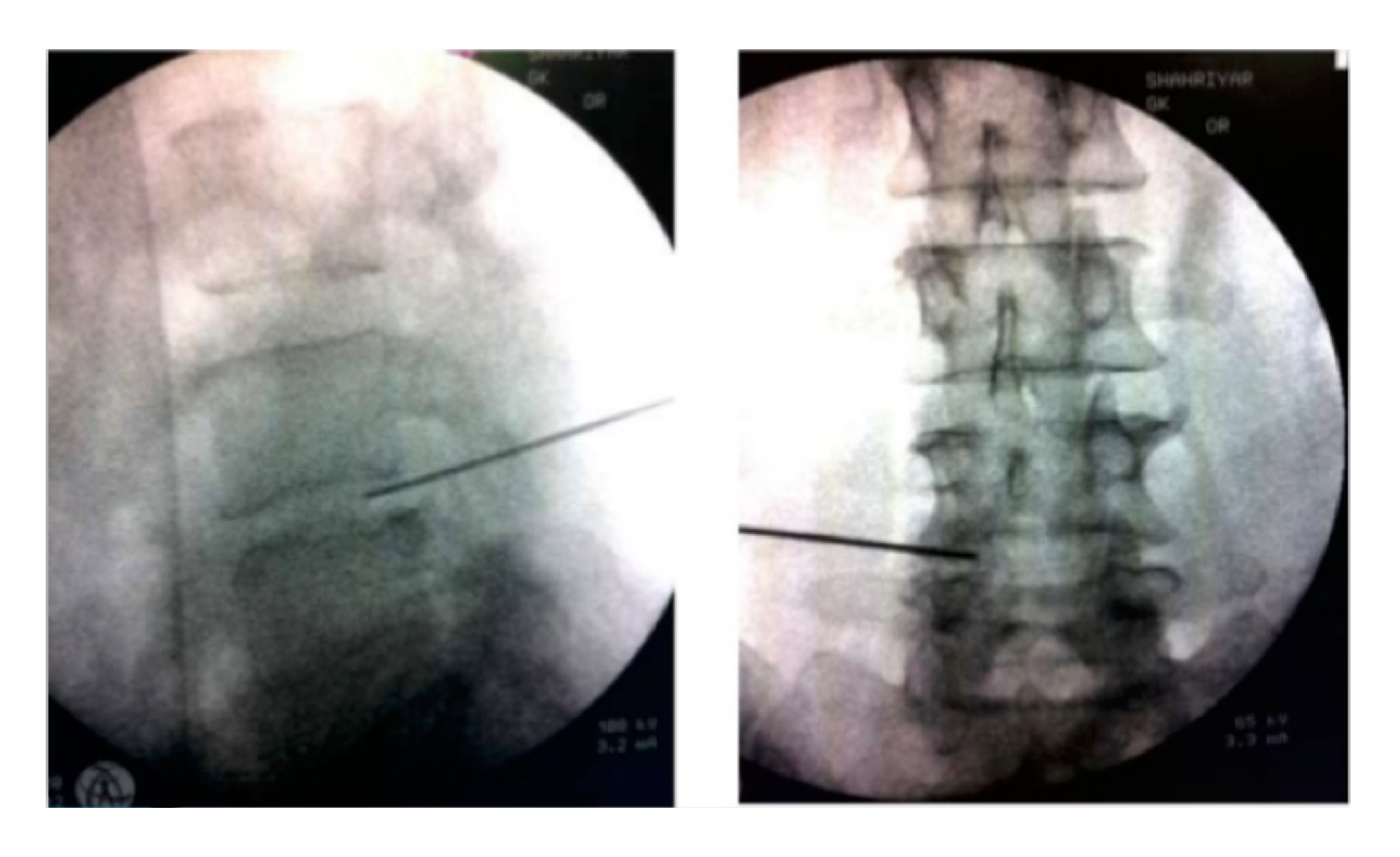
| Insert anesthesia needle (Kit ref. CBL18/20). Two AP and LL fluoroscopy controls will confirm the correct position of the needle, with which the required Local Anesthesia will also be performed. Penetrate the fibrous annulus and move to the center of the disc. |
 |
 |
|
| Remove the stylet from pink anesthesia needle, introducing the guidewire (Kit Ref. RK0518/38) to introduce the following cannulae. | 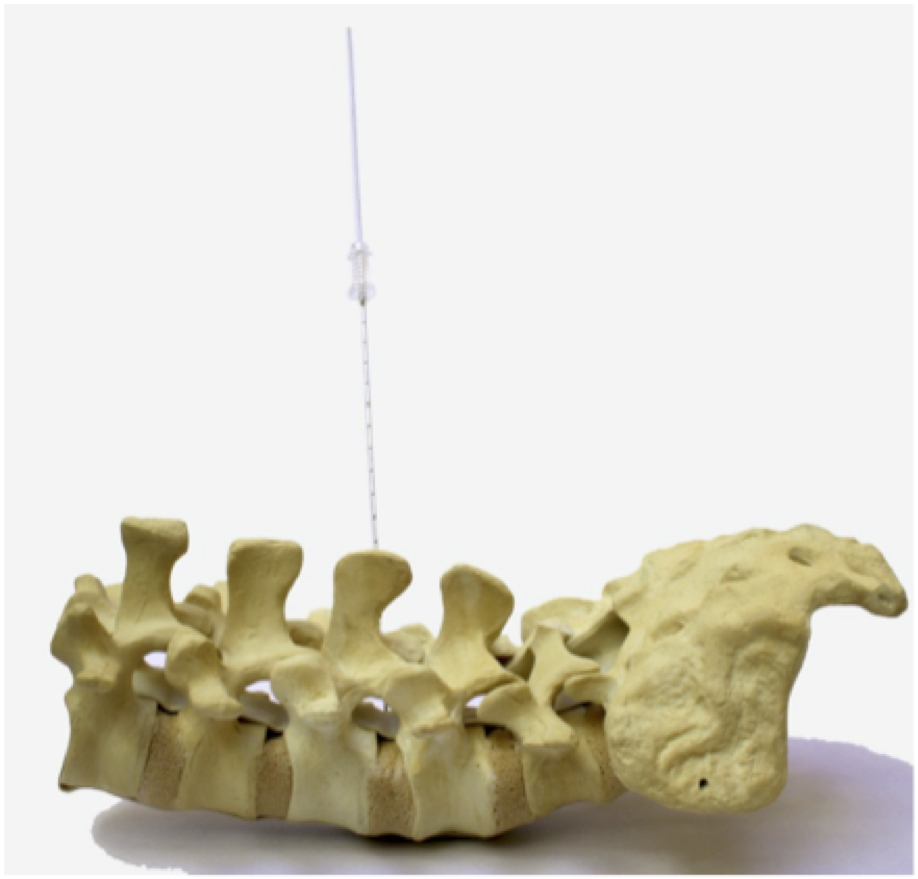 |
 |
Remove the anesthesia needle and slid the trocar cannula (Kit DBC13/19) along the guidewire, keeping the guidewire at the center of the disc. Extract trocar stylet and guidewire. |
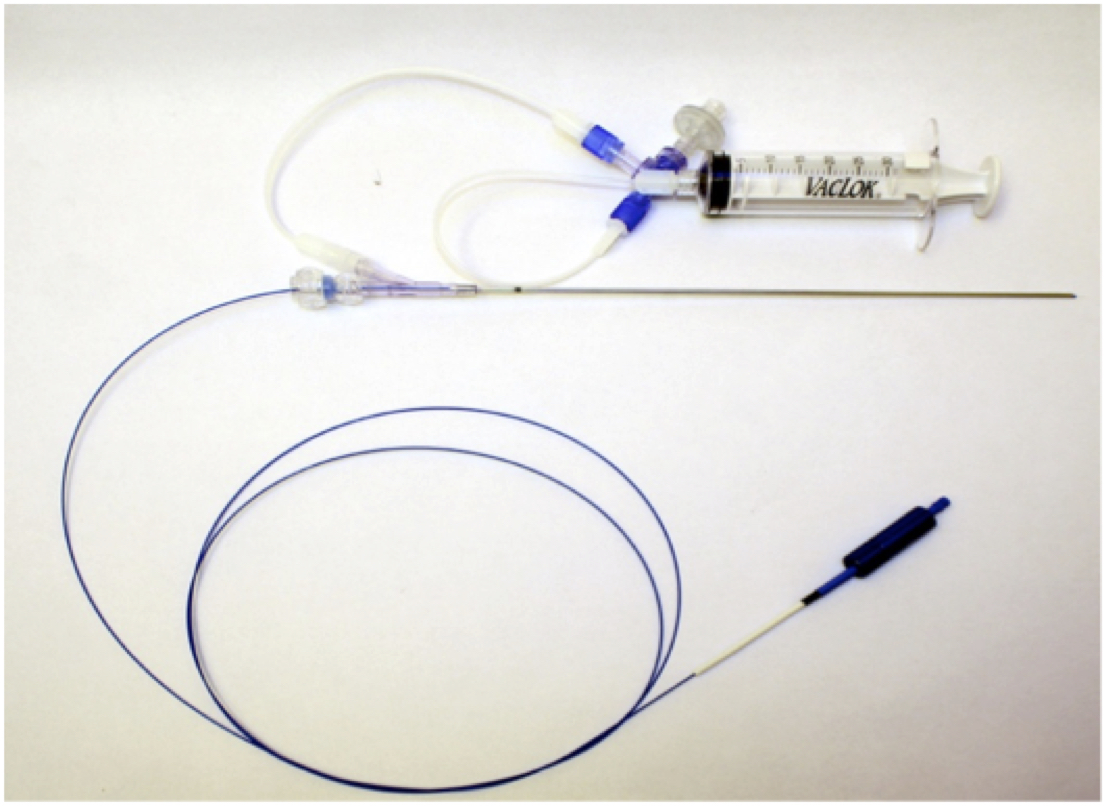 |
On the operating table, assemble the working cannula (Kit ref. DLC14/20) by inserting the Discolux® fiber (kit Ref. FBR08225) into the working cannula’s central hole, using the Fiber-Lock connector already positioned on the optical fiber. Connect vacuum system (Kit ref. CT40 and VS30), to the working cannula’s lateral hole. |
 |
The fiber-lock connector has 2 locking system: one blocks the fiber-lock to the working cannula’s central luer lock. |
| - The back one blocks the fiber in the desired position, to place the fiber’s tip 5/6 cm out from the end of the working cannula. Introduce the working cannula, previously assembled with the aspiration system and the laser fiber, inside the working cannula. |
 |
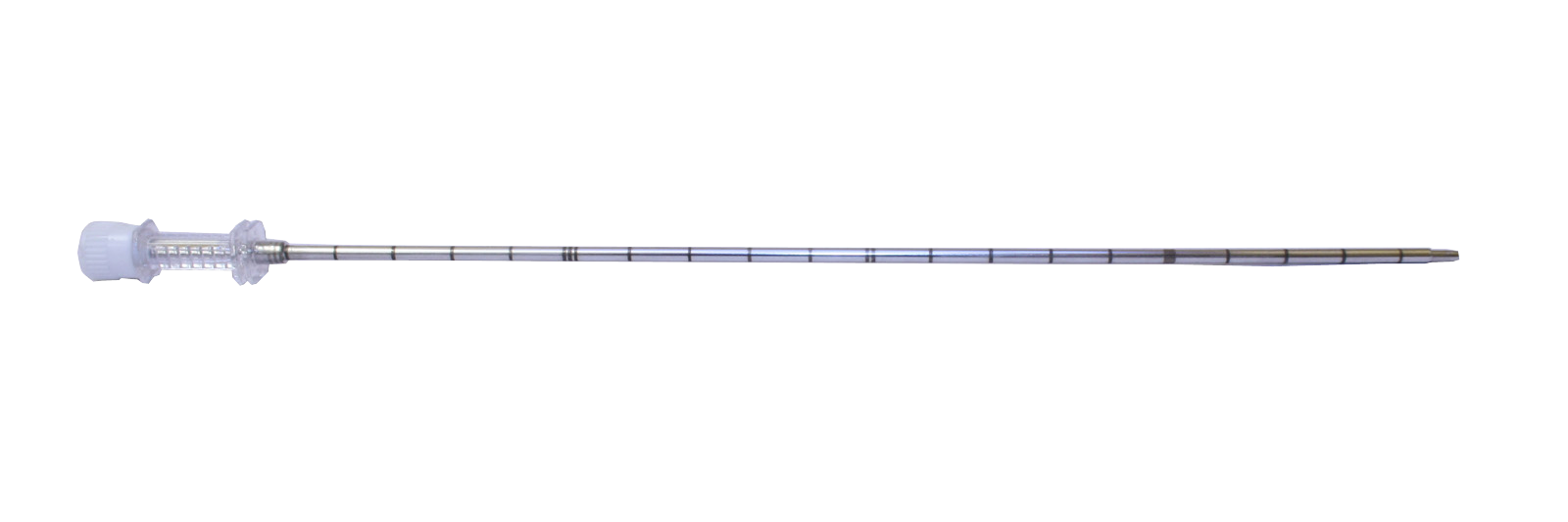 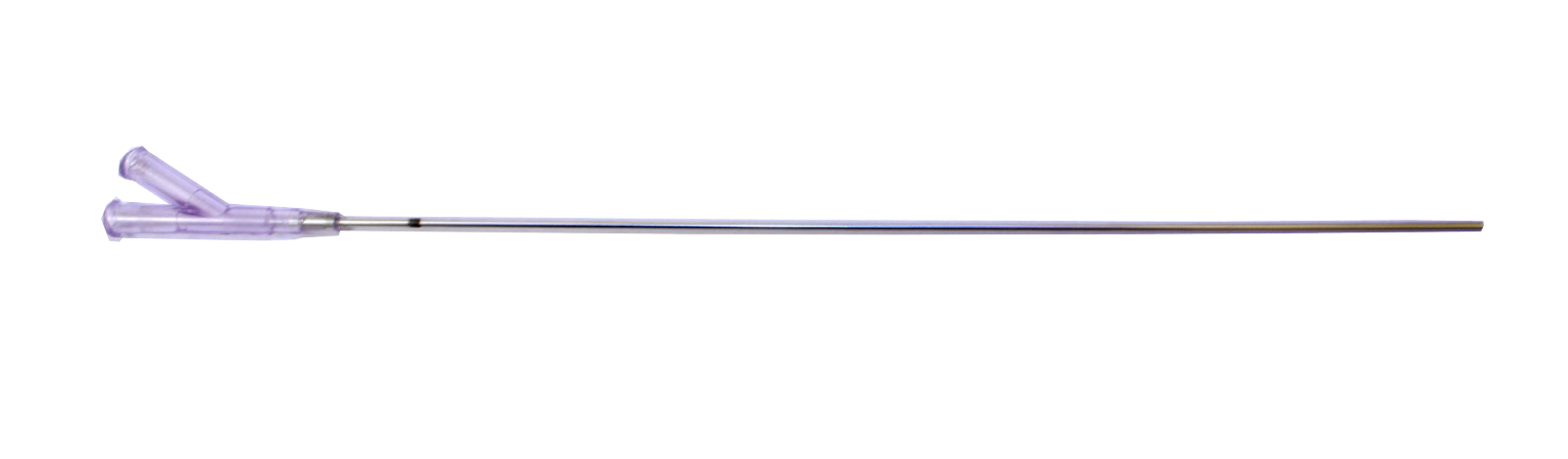 |
The Black Mark on the working cannula indicate the point where trocar and working cannula are at the same level and the laser fiber terminal enters into the disc. |
| At this point, with the optical fiber located at the center of the intervertebral disc, proceed with the laser treatment. | |
Laser Treatment:
Connect the fiber to the Discolux® laser generator; The whole procedure is handled by the Discolux® software and its total duration is 9 minutes, divided into 3 phases:
Each phase consists of 2 minutes (120 seconds) of continuous laser delivery with a power of 2.1 W, followed by 1 minute (60 Seconds) resting, which manually performs the suction 4 times through the dedicated Vacuum system (Kit Ref. VS30 and CT40).
| PHASE 1 | PHASE 2 | PHASE 3 | |||
| POWER | VACUUM | POWER | VACUUM | POWER | VACUUM |
| 120 sec. | 60 sec. | 120 sec. | 60 sec. | 120 sec. | 60 sec. |
| Apply pulsed light to the center of the disc | Apply the pulsed light to the first third of the disc | Apply pulsed light inside the disc protrusion close to the root |
|||
Ogni fase consiste in 2 minuti (120 Secondi) di erogazione laser continua con una potenza di 2.1 W, seguita da 1 minuto (60 Secondi) di riposo, in cui si esegue manualmente il Vacuum per 4 volte tramite il sistema di aspirazione dedicato (Kit Ref. VS30 e CT40).
 |
At the end of the procedure, you can check disc material removed through the vacuum system, directly in the working cannula.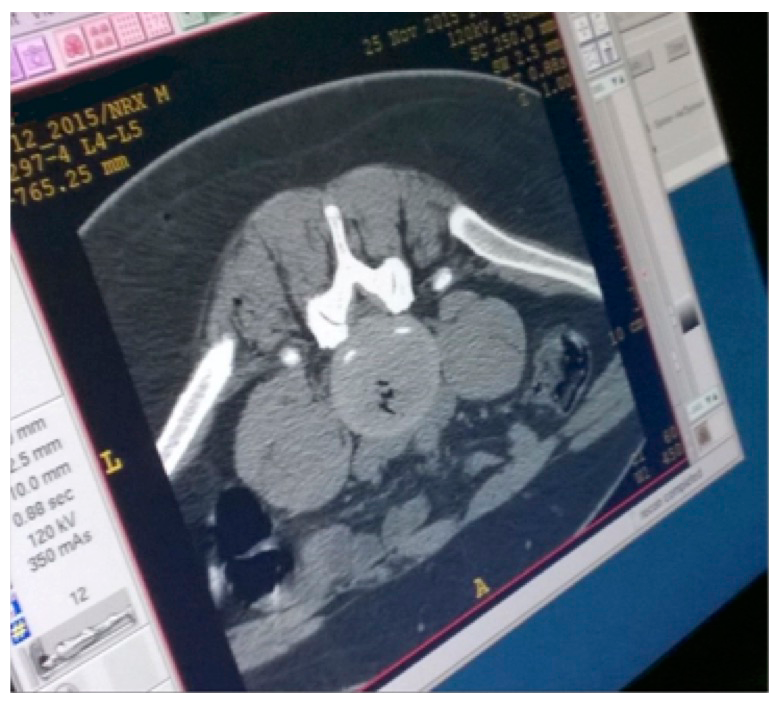 |
Certifications:
CE Discolux Laser |
CE Discolux Kit |
Bibliografy:
[1] Boswell MV, Trescot AM et al. Interventional techniques: evidence-based practical guidelines in the management of chronic spinal pain. Pain Physician 2007; 10:7-111.
[2] Gibby W. Automated percutaneous discectomy. In: Handbook of diagnostic and therapeutic spine procedures. A.L. Williams and F.R. Murtagh, Editors. St Louis: CV Mosby, 2002: 203-225.
[3]. Fenton DS, Czervionke LF. Discography. In: Handbook of diagnostic and therapeutic spine procedures. A.L. Williams and F.R. Murtagh, Editors. St Louis: CV Mosby, 2002: 167-199.
[4]. Fraser RD, Osti OL, Vernon-Roberts B. Discitis after discography. J Bone Joint Surg Br 1987; 69: 31.
[5]. Zeidman SM, Thompson K, Ducker TB. Complications of cervical discography: Analysis of 4400 diagnostic disc injections. Neurosurgery; 37: 414.
[6]. Simopoulos TT, Kraemer JJ, Glazer P, Bajwa ZH. Vertebral osteomyelitis: a potentially catastrophic outcome after lumbar epidural steroid injection. Pain Physician 2008 Sep-Oct; 11(5): 693-7.
[7] Smuck M, Benny B, Han A, Levin J. Epidural fibrosis following percutaneous disc decompression with coblation technology. Pain Physician. 2007 Sep; 10(5):691-6.
[8] Appleby D, Andersson G, Totta M. Metaanalysis of the efficacy and safety of intradiscal electrothermal therapy (IDET). Pain Med 2006; 4: 308-316.
[9] Gangi A, Dietemann JL, Ide C, Brunner P, Klinkert A, Warter JM. Percutaneous laser disc decompression under CT and fluoroscopic guidance: Indications, technique and clinical experience. Radiographics 1996; 16: 89-96.
[10] Connor PM, Darven BV. Cervical discography complications and clinical efficacy. Spine 1993; 18(14): 2035.
[11] Bogner EA. Past, present and future of therapeutic lumbar spine interventional procedures. Radiol Clin N Am 2009; 47(3): 411-419.
[12] Gangi A, Dietemann JL, Ide C, Brunner P, Klinkert A, Warter JM. Percutaneous laser disc decompression under CT and fluoroscopic guidance: Indications, technique and clinical experience. Radiographics 1996; 16: 89-96.
[13] Fenton DS, Czervionke LF. Intradiscal electrothermal therapy. In: Image guided spine intervention. Saunders 2003; 257-285.
[14] Fenton DS, Czervionke LF. Discography. In: Handbook of diagnostic and therapeutic spine procedures. A.L. Williams and F.R. Murtagh, Editors. St Louis: CV Mosby, 2002: 167-199. [15] Eckel, TS. Intradiscal electrothermal therapy. In: Handbook of diagnostic and therapeutic spine procedures. A.L. Williams and F.R. Murtagh, Editors. St Louis: CV Mosby, 2002: 229-244.